The essential thrombocythemia is a blood disease characterized by an increased production of platelets. According to current knowledge, it is genetically determined. Thrombosis is common.
What is essential thrombocythemia?
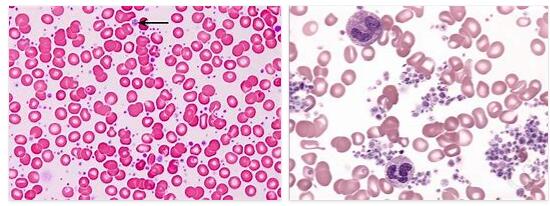
According to eshaoxing.info, essential thrombocythemia is a myeloproliferative neoplasia (MPN). This leads to an increased formation of blood platelets. The term “essential” means that the increased platelet production is not a side effect of another blood disorder, but the primary symptom. Usually between 150,000 and 450,000 platelets per microliter of blood are found in the blood. If the platelet count rises above 450,000 microlitres, the values are increased, but without symptoms.
If the number exceeds 600,000, increased thrombus formation can occur, which is associated with the formation of thromboses and microcirculation disorders. If the value is above 1,000,000 platelets per microliter, an increased tendency to bleeding becomes more prominent instead of thrombosis. The task of the blood platelets is to seal the blood vessel by clumping together in the event of an injury, thereby forming a blood clot that quickly dissolves again after it has healed.
The increased number of platelets can lead to large blood clots, which clog the blood vessels. However, even higher platelet concentrations ensure the absorption of coagulation factors and thereby increase the bleeding tendency again. Women are more often affected by the disease than men. Life expectancy is normal for the mild form of ET.
Causes
Like all myeloproliferative neoplasms, essential thrombocythemia is genetic. However, despite their genetic makeup, the disease does not occur in every patient. The severity of the disease is also different for different people. The genetic background has not yet been fully elucidated. In recent years, however, three different mutations have been identified for this disease. In half of all cases there is a mutation in the tyrosine kinase JAK2.
It is the JAK2 mutation V617F. With this mutation, the tyrosine kinase JAK2 remains permanently active and causes the constant production of platelets. However, it was found that the JAK2 mutation-V617F also exists in other MPNs such as polycythemia vera or osteomyelofibrosis. One percent of the cases have a mutation in the gene for the thrombopoietin receptor MPL. This permanently stimulates the blood stem cells concerned to grow.
In 70 percent of all diseases without the JAK2 mutation-V617F, the CALR gene, which codes for the calreticulin protein, is changed. Interestingly, the JAK2, MPL, and CALR mutations never appear together. It can therefore be assumed that at least three different mutations must be responsible for the same clinical picture.
Symptoms, ailments & signs
Essential thrombocythemia occurs in three different forms. The development of the symptoms depends largely on the concentration of platelets. In many cases the disease is symptom-free. When symptoms occur, they are usually microcirculatory disorders with increased blood pressure or functional disorders. Thromboses, heart attacks, strokes or embolisms can occur as complications. In an embolism, a blood clot breaks up and blocks the corresponding blood vessel.
On the other hand, insufficient blood circulation can occur in different parts of the body such as the legs or the head (emptiness in the head). For example, there is severe pain in the legs when walking. If the platelet count has risen above one million per microliter of blood, there is again an increased tendency to bleed. A third of patients have no symptoms. The average life expectancy in these cases corresponds to that of the normal population.
Diagnosis
The diagnosis of essential thrombocythemia is now usually made as part of a routine examination, as the disease is often symptom-free. Increased platelet counts are found. The cause of the increased values must then be further clarified. Because high platelet concentrations can also occur in many other diseases. These include iron deficiency, infections or certain tumors.
Various criteria must be present to uniquely identify an ET. The number of leaflets is consistently above 600,000 per microliter. A bone marrow histology will find enlarged, mature megakaryocytes. Furthermore, the typical mutations for ET must be diagnosed. Since a JAK2 mutation is also present in other MPNs, various other blood diseases must be ruled out.
Complications
With essential thrombocythemia, there is an increased formation of platelets in the blood. This creates the risk of a circulatory disorder. The result is an increased tendency of the blood to clot, which can lead to serious complications. Local blood clotting occurs again and again, which leads to the formation of a blood clot (thrombus).
Both the venous and arterial blood systems can be affected. In ET there is a particular risk of thrombosis of the deep veins in the legs (phlebothrombosis), the hepatic veins (Budd-Chiari syndrome) and the abdominal veins, especially the portal vein. A dreaded complication is thromboembolism, in which a thrombus is carried away by the bloodstream and closes a part or branch of a vessel.
If the venous system is affected, pulmonary embolism can occur. The consequences of an arterial thromboembolism are splenic infarction, heart attack and stroke. Microembolism in the brain can lead to a transient ischemic attack (TIA) with temporary symptoms that resemble a stroke. The duration of the neurological disorder is usually limited to one to two hours.
In addition, the essential thrombocythemia can pass into another disease from the group of myeloproliferative neoplasms. In most cases, myelofibrosis or polycythemia vera will develop. The development of acute myeloid leukemia is very rare.
When should you go to the doctor?
A doctor must always be consulted with this disease. This avoids serious complications which, in the worst case scenario, can lead to death. A doctor should always be consulted if the person concerned has been suffering from high blood pressure for a long period of time. This can also lead to the formation of thromboses on the body. The disease can also cause a stroke or a heart attack. If this happens, an emergency doctor must be called immediately. In addition, mouth-to-mouth resuscitation and cardiac massage must be carried out until the emergency doctor arrives.
The affected person should be brought into a stable side position, if possible. A visit to the doctor is also necessary if the patient suffers from disorders of the blood circulation, which can usually be seen as impaired sensitivity or paralysis. If the disease does not lead to complaints or symptoms, no treatment is usually necessary. The diagnosis can be made by a general practitioner. However, further treatment depends heavily on the underlying disease and is carried out by a specialist. In most cases, this does not reduce the patient’s life expectancy.
Treatment & Therapy
Treatment for essential thrombocythemia depends on the severity of the disease. High-risk patients with a number of leaflets above 1500,000 per microliter or who are prone to severe thrombosis or bleeding must always be treated with chemotherapy with hydroxycarbamide, anagrelide or alpha interferon. Anagrelide inhibits the growth of megakaryocytes in the bone marrow. The drugs hydroxycarbamide or alpha interferon suppress the constant formation of platelets.
Which drug should be used must be decided on a case-by-case basis. A medium risk is present if there is already cardiovascular disease of another origin, diabetes mellitus or hypercholesterolemia. Chemotherapy should be weighed up individually, taking into account the advantages and disadvantages. The blood thinner acetylsalicylic acid may possibly be used in low doses.
If the platelet count is below 1,500,000 per microliter, the patient is under 60 years old and there are no or only minor symptoms, therapy is limited to regular exercise, weight reduction, avoiding long periods of sitting and dehydration, and observing the early symptoms of thrombosis.
Outlook & forecast
There is no cure for essential thrombocythemia. The cause of the disease is based on a mutation in the genes. The genetics of humans may not be changed due to legal requirements by scientists and medical professionals. Treatment can therefore only be given symptomatically. As soon as the therapy is interrupted, the symptoms reappear immediately. Due to this situation, long-term therapy is necessary to improve health. If left untreated, the affected person is at risk of developing a thrombus. There is thus a potential danger to life.
The prognosis also depends on the severity of the disease. In mild cases, medication is given. These monitor and regulate the formation of blood cells. The symptoms are relieved. The effectiveness of the preparations is checked in regular check-ups.
In severe cases, treatment with chemotherapy is indicated. This is associated with various side effects. The quality of life is impaired and everyday obligations can often not be fulfilled. Nevertheless, according to the current medical status, this is the only way to extend the life span. In order to reduce the side effects of the treatment, the affected person should be careful to lead a healthy lifestyle. Long periods of sitting should be avoided, a balanced diet supports the organism and sufficient fluids should be consumed.
Prevention
In general, essential thrombocythemia cannot be prevented because it is genetic. To avoid the onset of symptoms in low-risk patients, a healthy lifestyle with plenty of exercise, a healthy diet, and adequate hydration is recommended.
Aftercare
In some cases, the person affected has only very limited options or measures of follow-up care at their disposal. First and foremost, the disease must be recognized and treated early so that other complications or complaints do not occur. A cure can only occur if treatment is started early. However, since the disease is genetic, only purely symptomatic treatment can be carried out.
If the person concerned wishes to have children, genetic counseling can also be carried out. This may prevent the disease from being passed on to descendants. Self-healing does not occur with this disease. Since this disease can very often lead to the development of a thrombosis, regular examinations should be carried out by a doctor.
Measures must also be taken to prevent cancer so that tumors can be detected and removed at an early stage. In general, a healthy lifestyle with a healthy diet has a positive effect on the further course of this disease. In many cases, however, the life expectancy of the person affected is reduced by this disease despite treatment. Further aftercare measures are not available to the affected person.
You can do that yourself
Patients with essential thrombocythemia should eat a balanced and healthy diet to maintain good health. The own weight should be within normal weight according to the guidelines of the BMI. Avoid being overweight. A vitamin-rich diet that contains a lot of iron is recommended. In addition, the intake of the recommended daily amount of fluid must be observed, as the body must be protected from dehydration.
Adequate exercise, long walks and regular exercise also help to improve health. When choosing sports, it is important that a holistic exercise takes place and that the body is not overburdened. Sports like swimming or jogging are advisable. These stimulate the cardiovascular system, but do not overwhelm the organism.
Rigid postures or long periods of sitting and standing should be avoided as a matter of principle. In everyday life, the body position must be changed at regular intervals. Slight loosening can be exercised by stretching and stretching movements. The circulation can be stimulated with a few counter or compensatory movements. The consumption of stimulants such as nicotine or alcohol is prohibited. Regular participation in check-ups is helpful. The older a patient, the shorter the time intervals should be.